Kids Emergency Department: Fast Help for Your Child’s Urgent Needs

Why Emergency Care for Kids Matters More Than You Think
As a parent, your child’s safety and well-being are your top priorities. From the moment they are born, you dedicate yourself to protecting them. But what happens when the unexpected occurs? A sudden high fever, a fall from the monkey bars, or a chipped tooth can send any parent into a panic. In these moments, knowing how to react quickly and appropriately is not just helpful—it can be life-saving. Emergency care for kids is a critical aspect of parenting that every caregiver should be prepared for, because accidents and illnesses don’t operate on a 9-to-5 schedule.
The statistics are sobering: injuries are the leading cause of death among children in the United States. Every year, millions of children are treated in emergency departments for injuries, many of which are preventable. Beyond accidents, sudden illnesses can escalate quickly in young children. Understanding the signs of a true emergency and knowing where to seek the right level of care can make all the difference in the outcome.
This guide is designed to empower you with the knowledge to act confidently in a crisis. We’ll explore the key differences between visiting your pediatrician, an urgent care center, or the emergency room. We’ll also cover essential first-aid tips and how to prepare your family for a medical emergency, including dental-specific issues. I’m Dr. Risha Khan, and as a mother of two young children myself, I understand the anxiety that comes with a child’s health scare. Through my decade of experience in dentistry and pediatric care at Arista Dental Care of Edmonds, I’ve guided countless families through dental emergencies and helped them understand when urgent emergency care for kids is truly necessary. Let me walk you through everything you need to know to act quickly and confidently when your child needs help.
Recognizing a True Emergency: When to Act Fast
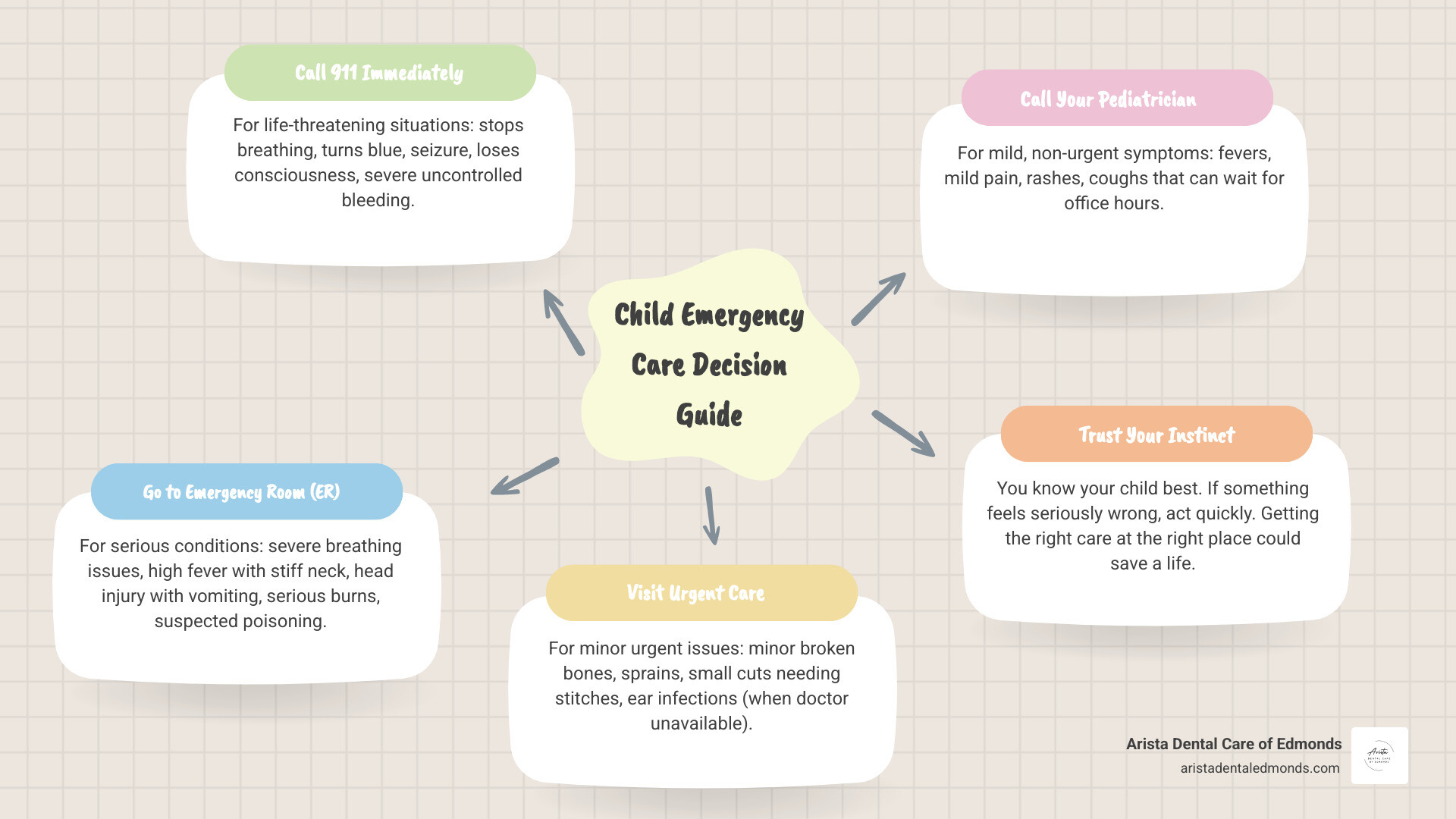
When your child is unwell or injured, the first and most crucial step is to assess the situation and determine if it’s a true medical emergency. This can be a frightening moment for any parent, but understanding the signs of distress can empower you to act decisively. We always say, “you know your child best,” and trusting your parental instinct is incredibly important. If something feels seriously wrong, it often is. A child who is unusually lethargic, inconsolable, or showing a sudden, drastic change in behavior warrants immediate medical attention.
Signs of severe distress can include rapid, labored breathing, changes in consciousness (such as unusual sleepiness or difficulty waking up), or severe, persistent pain that doesn’t subside. These are moments when prompt action is not just helpful, it’s essential for your child’s well-being. For a comprehensive guide on recognizing these critical moments, we recommend reviewing resources like When to Get Emergency Care for Your Child.
Key Signs Your Child Needs Emergency Care for Kids
It’s natural to feel overwhelmed when your child is sick or injured. To help you make the best decision, here are key signs that indicate your child requires immediate emergency care for kids:
- Uncontrolled Bleeding: If your child has a deep cut or injury that is bleeding heavily and doesn’t stop after 5-10 minutes of applying firm, direct pressure, it’s an emergency. A cut that is gaping open, even if not bleeding profusely, may also require stitches and should be seen by a medical professional.
- High Fever with Other Symptoms: A high fever, especially when accompanied by a stiff neck, unusual sleepiness, a rash that doesn’t fade when pressed, or confusion, can indicate a serious infection like meningitis and requires immediate medical attention. For infants under 3 months, any fever of 100.4°F (38°C) or higher is a medical emergency.
- Seizures: If your child is having a seizure, particularly one lasting more than 5 minutes or if it’s their first seizure, they need emergency care. During a seizure, ensure their safety by placing them on their side on the floor, away from any hard or sharp objects. Do not put anything in their mouth or try to restrain them. Time the seizure and call 911.
- Major Injuries: This includes suspected broken bones (especially if the bone is protruding through the skin or the limb is at an odd angle), significant head trauma with loss of consciousness (even for a moment), persistent vomiting, or confusion, and any injury to the neck or spine.
- Severe All-ergic Reactions (Anaphylaxis): Signs like difficulty breathing, wheezing, swelling of the face, lips, or tongue, hives spreading rapidly over the body, or a sudden drop in blood pressure after exposure to an allergen indicate a life-threatening reaction. Use an epinephrine auto-injector if available and call 911 immediately.
- Dehydration Signs: In infants and young children, dehydration can become serious quickly. Signs include a dry mouth and tongue, no tears when crying, no wet diapers for 6-8 hours (or very dark, strong-smelling urine), sunken eyes or a sunken soft spot (fontanelle) on an infant’s head, and extreme lethargy or irritability. These symptoms require urgent medical evaluation.
- Head Trauma with Vomiting: If your child hits their head and subsequently vomits multiple times, loses consciousness, becomes unusually drowsy or confused, or complains of a severe headache, seek emergency care immediately. These could be signs of a concussion or more serious brain injury.
For more detailed information on recognizing these critical situations, we find the American Academy of Pediatrics’ resource, When Your Child Needs Emergency Medical Services, to be incredibly helpful.
When to Call 911 Immediately
There are certain situations where every second counts, and calling 911 (or your local emergency number) for an ambulance is the fastest and safest way to get your child the help they need. Paramedics can begin life-saving treatment on the way to the hospital. Our priority is always to ensure your child receives the most appropriate and timely care.
You should call 911 for your child if they:
- Are not breathing or turn blue/purple/gray. This is a sign of severe respiratory distress or cardiac arrest.
- Are choking and you cannot clear their airway with back blows or abdominal thrusts (Heimlich maneuver).
- Are unconscious or unresponsive and cannot be woken up.
- Are having a severe seizure (especially if it’s their first, lasts longer than 5 minutes, or they don’t recover quickly).
- Have a severe burn that is large (covering more than 10% of their body), deep, or involves the face, hands, feet, or genitals.
- Might have a neck or spine injury (e.g., after a fall from a height, a car accident, or a diving incident). It is crucial not to move them unless they are in immediate danger, as this can cause permanent paralysis.
- Have ingested a poison, chemical, or unknown substance and are showing severe symptoms like loss of consciousness, difficulty breathing, or seizures. (Always call Poison Control first at 1-800-222-1222 for suspected poisoning if they are stable, but if severe symptoms are present, call 911).
- Have bleeding that cannot be stopped with 10-15 minutes of firm, direct pressure.
- Are involved in a serious accident (e.g., car crash, fall from a significant height) and are seriously injured or unconscious.
- Show signs of a severe allergic reaction (anaphylaxis) with trouble breathing, swelling of the face or tongue, or collapse.
If you’re ever unsure whether your child’s condition warrants a 911 call, it’s always best to err on the side of caution. As parents and healthcare providers, we understand that panic can set in, but a quick call can bring trained professionals to your side.
Where to Go: ER, Urgent Care, or Your Doctor?
Deciding where to take your child when they’re sick or injured can feel like navigating a maze. Should you head straight to the emergency room, visit an urgent care clinic, or call your pediatrician? Each option serves a different purpose, and knowing the distinction can ensure your child gets the right care efficiently, potentially saving you time, stress, and money. Treatment in an emergency department can cost 2 to 3 times more than the same care in your provider’s office, and wait times can be significantly longer for non-critical issues.

When considering your options, it’s also helpful to think about the geography. For families in Edmonds, Shoreline, Lynnwood, or Mountlake Terrace, we have a variety of facilities available. While a children’s hospital emergency department offers specialized pediatric care with staff and equipment custom for kids, general hospital ERs are also equipped to handle severe emergencies. The key is understanding the severity of your child’s condition to choose the most appropriate setting.
Emergency Room (ER) vs. Urgent Care Clinic
Understanding the difference between an Emergency Room (ER) and an Urgent Care Clinic is crucial for making informed decisions about your child’s health. Both provide immediate medical attention, but for very different types of situations. The ER is for life-threatening emergencies, while urgent care is for issues that are not life-threatening but can’t wait for a regular doctor’s appointment.
Here’s a breakdown to help you decide:
| Feature | Emergency Room (ER) – | Urgent Care Clinic – |
|---|---|---|
| Purpose | For life-threatening emergencies and severe injuries. – Urgent Care Clinic – – | |
| – Conditions Treated | Severe bleeding, difficulty breathing, chest pain, loss of consciousness, major trauma, high fever with confusion, severe allergic reactions, suspected poisoning, broken bones with deformity. – Minor illnesses and injuries that are not life–threatening but require prompt attention. Examples include colds, flu, ear infections, minor cuts, sprains, and mild asthma attacks. – | |
| – Hours of Operation | 24/7, including holidays. – Typically extended hours, including evenings and weekends, but not always 24/7. | |
| – Equipment & Staff | Equipped for life-threatening conditions with specialists, advanced imaging (CT scans, MRI), and surgical capabilities. – Equipped for common illnesses and minor injuries. May have X-ray capabilities but not advanced imaging. Staffed by general practitioners, physician assistants, and nurse practitioners. – | |
| – Cost | Significantly higher due to the level of care and resources available. – More affordable than an ER visit for similar services. – | |
| – Wait Times | Can be very long for non-critical issues as life-threatening cases are prioritized. – Generally shorter wait times compared to the ER. – |
The Role of Telehealth and Your Pediatrician
Telehealth has become an invaluable resource for parents. For non-urgent concerns, a virtual consultation can save you a trip to the clinic. Many pediatric practices, including specialists, now offer video appointments to discuss symptoms, provide advice, and even prescribe medication when appropriate. This is ideal for conditions like mild rashes, colds, or follow-up questions. However, it’s important to recognize the limitations of telehealth; a physical examination is often necessary for an accurate diagnosis.
Your primary pediatrician should always be your first point of contact for non-emergency health concerns. They know your child’s medical history, vaccination records, and any pre-existing conditions. Building a long-term relationship with a pediatrician ensures continuity of care, which is crucial for your child’s overall health and development. They can manage chronic conditions, track developmental milestones, and provide guidance on everything from nutrition to behavior. Many offices have an after-hours line to help you decide if a trip to the ER or urgent care is necessary. For families in our community, resources like the Thames Valley Family Health Team can also provide guidance and support in navigating healthcare options.
Edmonds Dentist

21727 76th Ave W Ste G, Edmonds, WA 98026
(425) 967-7272
info@aristadentaledmonds.com
Edmonds Dentist
21727 76th Ave W Ste G, Edmonds, WA 98026(425) 967-7272
info@aristadentaledmonds.com